When prescribing pain medications you must also consider the side effects that those medications may have on your patient such as nausea, constipation, rash, etc.
We will talk about anti-emetics today.
There are many classes of anti-emetics to consider. Most services have their favorites, but due to patient allergies and the ineffectiveness of some medications on some patients - it is good to have a few back-ups in mind to try. You can also consult the pharmacy team that you work with for additional advice. This list is not comprehensive.
Dopamine antagonist:
Prochlorperazine (good for opiod related nausea), Metoclopramide, Haloperidol
5HT3 antagonists:
Ondansetron* (PO and IV)
Antihistamines:
Diphenhydramine**
Anticholinergics:
Scopolamine
Antipsychotics:
Olanzapine
*can lead to headaches and constipation
**can be sedating
Source: MPR http://www.empr.com/antiemetic-treatments/article/125873/
False Starts, Stumbles, and Spectacular Finishes Encountered on the PA Path...
Showing posts with label medicine. Show all posts
Showing posts with label medicine. Show all posts
4.20.2014
1.14.2014
What is a WADA exam?
What is a WADA exam?
A WADA exam is also known as an intracarotid amytal test. It
is one of the “non-invasive” tests used to determine which hemisphere is
language dominant in epileptic patients and also assess the ability of the non-affected
side to maintain memory when isolated. For example, if you were to remove the R
hippocampus – could the L side support language and memory alone?
No test is perfect... here are a couple of the WADA Shortcomings:
- If patient has a high flow AVM – reading can be inaccurate
- A portion of the hippocampus that you are trying to shut down could get its blood supply from posterior circulation making it hard to tell how accurately the patient will respond with full resection.
How is it done?
- Get angiogram (to assess cross flow – which is a contraindication to shutting down the side of primary supply)
- Cath ICA (usually start on lesion side)
- Ask pt to hold opposite arm in the arm as amobarbital is rapidly injected into the ICA
- What should happen? An almost immediate flaccid exam of the arm that begins to wear off in about 8 minutes. If it wears off faster (around 2 minutes) you may think about a high flow AVM.
- Assess language by asking pt to name objects and remember them
- Assess memory by asking pt to recall as many of the objects as possible 15 minutes later
- Procedure can be repeated on the other side if needed

Photo source: http://www.instantanatomy.net/headneck/vessels/articinskull.html
Source: Handbook of Neurosurgery, Greenberg 6th Ed
8.01.2013
Passing the Time on the T with JAAPA
So the PA Journal (JAAPA) now has an application for the iPad. It has been out for a while now and I really like it! I download the most recent journal and am able to read it on the T on the way to work. It is great... it helps me keep up on the newest issues and clinical articles. The only downside is that it is only for the iPad currently... sorry no iPhones or iPods.
If you are an AAPA member, you get the journal for free along with the free CMEs in each issue.
Down load it at the Apple App Store: Journal of the American Academy of Physician Assistants
If you are an AAPA member, you get the journal for free along with the free CMEs in each issue.
Down load it at the Apple App Store: Journal of the American Academy of Physician Assistants
7.11.2013
Oliguria
As always... back to the basics:
What is oliguria?
Low urine output (UOP)
What is "normal" adult UOP?
About 30cc/hr
How might you write a post op floor order for this?
"call house officer if 2 hour UOP is < 60cc"
What are the possible causes?
Think pre renal/renal/post renal causes
What is the most common cause?
Pre renal!
What is oliguria?
Low urine output (UOP)
What is "normal" adult UOP?
About 30cc/hr
How might you write a post op floor order for this?
"call house officer if 2 hour UOP is < 60cc"
What are the possible causes?
Think pre renal/renal/post renal causes
What is the most common cause?
Pre renal!
3.06.2013
Hematuria Workup
A diagnostic algorithm to consider when working up hematuria...
Source: Ferri's Best Test: A practical guide to clinical lab and medicine diagnostic imaging, Fred Ferri
click on picture to enlarge
Source: Ferri's Best Test: A practical guide to clinical lab and medicine diagnostic imaging, Fred Ferri
3.03.2013
IV Therapy Complications
"Let's give him/her some IV fluids." Seems like a simple enough order. IV therapy is part of medicine, but it is not without risks. It is important to know the risks so that you know what complications to look for in the seconds, hours, days after an IV has been started.
Thrombophlebitis - usually manifests with erythema, inflammation, and/or pain at the IV site (think about changing the IV q3 days to help prevent this)
Infiltration - this happens when whatever you are giving through the IV (meds/fluids) starts to leak into the surrounding tissue (this can cause a big problem - compartment syndrome - if the volume is large enough)
Blockage - something, a blood clot for example, can clog the IV making it unusable (flushes can help minimize the risk of this)
Air embolus
Thrombophlebitis - usually manifests with erythema, inflammation, and/or pain at the IV site (think about changing the IV q3 days to help prevent this)
Infiltration - this happens when whatever you are giving through the IV (meds/fluids) starts to leak into the surrounding tissue (this can cause a big problem - compartment syndrome - if the volume is large enough)
Blockage - something, a blood clot for example, can clog the IV making it unusable (flushes can help minimize the risk of this)
Air embolus
Source: Step up to Medicine 2nd ED Agabegi and Agabegi
Pic source: http://en.wikipedia.org/wiki/Intravenous_therapy
2.16.2013
Carpal Tunnel
Carpal Tunnel
See below for the answers.
What nerve is compressed in carpal tunnel?
What population is it most commonly seen in?
What are typical signs and symptoms?
Where is the anatomical location of the "carpal tunnel"?
Work up?
Treatment?
What nerve is compressed in carpal tunnel?
Median nerve
What population is it most commonly seen in?
Women 30-50 years old
What are typical signs and symptoms?
Wrist pain - numbness/tingling of thumb
Pain exacerbated with activities of wrist flexion
May awaken pt at night
Thenar atrophy
Where is the anatomical location of the "carpal tunnel"?
Between the carpal bones and the flexor retinaculum
Work up?
Clinical exams: Tinel's sign and Phalen's sign
EMG/nerve conduction study
Treatment?
neutral wrist orthosis
modification of activities that irritate
NSAIDs for inflammation control
steroid injections
surgery
Source: First Aid for the Wards (Le, Bhushan, Skapik)
Photos: www.methodistorthopedics.com , http://en.wikipedia.org/wiki/File:Carpal_Tunnel_Syndrome,_Operation.jpg
See below for the answers.
What nerve is compressed in carpal tunnel?
What population is it most commonly seen in?
What are typical signs and symptoms?
Where is the anatomical location of the "carpal tunnel"?
Work up?
Treatment?
What nerve is compressed in carpal tunnel?
Median nerve
What population is it most commonly seen in?
Women 30-50 years old
What are typical signs and symptoms?
Wrist pain - numbness/tingling of thumb
Pain exacerbated with activities of wrist flexion
May awaken pt at night
Thenar atrophy
Where is the anatomical location of the "carpal tunnel"?
Between the carpal bones and the flexor retinaculum
Work up?
Clinical exams: Tinel's sign and Phalen's sign
EMG/nerve conduction study
Treatment?
neutral wrist orthosis
modification of activities that irritate
NSAIDs for inflammation control
steroid injections
surgery
Source: First Aid for the Wards (Le, Bhushan, Skapik)
Photos: www.methodistorthopedics.com , http://en.wikipedia.org/wiki/File:Carpal_Tunnel_Syndrome,_Operation.jpg
2.01.2013
Repleting K+
Electrolyte imbalances are something that you see a lot on your rotations - especially in internal medicine, emergency medicine, and surgery.
When thinking about repleting a potassium deficiency consider the following:
*This is not meant to substitute for clinical judgement, just suggestions to think about when treating K+ deficiencies in your patients.
Source:
http://www.eric.vcu.edu/home/curriculum/print/Intern_Ward_Survival_Guide_2009.pdf
http://www.surgicalcriticalcare.net/Guidelines/electrolyte_replacement.pdf
photo: http://mattrosenart.deviantart.com/art/Potassium-195578504
When thinking about repleting a potassium deficiency consider the following:
- Goal is of K is greater than 4 in any pt with active cardiac problems
- If your pt has nl renal function: 10mEq of KCl (IV or PO) will increase serum K by about 0.1mEq/L (so if your pt is at 3.6, about 40 mEq of KCl should help correct your patient)
- Don't replete if patient is on dialysis (consult the dialysis team)
- f your pt has compromised renal function: divide the mEq of normal repletion by the pt's Cr (example: pt has Cr of 3, then you use 1/3 of the nl repletion amount - so instead of 9mEq, you'd use 3mEq)
- PO can cause nausea
- IV can be painful
- Typical combos: 10mEq/100cc or 10mEq/50cc (peripheral IV) and 20mEq/50cc (central line)
- Be careful when repleting its with renal insufficiency or in pts with high risk of tumor lysis
*This is not meant to substitute for clinical judgement, just suggestions to think about when treating K+ deficiencies in your patients.
Source:
http://www.eric.vcu.edu/home/curriculum/print/Intern_Ward_Survival_Guide_2009.pdf
http://www.surgicalcriticalcare.net/Guidelines/electrolyte_replacement.pdf
photo: http://mattrosenart.deviantart.com/art/Potassium-195578504
11.01.2012
Approach to Volume Disorders, Part 2
Assessing Volume Status
Source: Step up to Medicine (Agabegi and Agabegi)
 |
| http://cutcaster.com/photo/100023974-IV-Drip/ |
- Track ins and outs (Is & Os) - this is not an exact science because you can't exactly measure insensible losses, but it will give you an idea of the volume status
- Normal urine output of an adult = 1mL/kg per hr
- Skin turgor and mucous membranes are difficult to assess and are not always reliable
- Daily wts are a good way to assess volume trends
- Don't lose sight of the BIG PICTURE. What is the overall health of your patient?
- Pts with: fever, burns, open wounds have a higher insensible loss
- For each degree over 37 degree C, estimate an increase in loss of 100mL/ day
- Pts with CHF may have pulmonary edema so pay close attention to their volume status
- Pts with end stage renal dz are prone to hypervolemia
- Pts with hypOalbuminemia tend to "3rd space" fluids out of vasculature and are therefore total body hypervolemic, but intra-vascularly depleted
Source: Step up to Medicine (Agabegi and Agabegi)
10.30.2012
Approach to Volume Disorders, Part 1
Volume disorders are tough. They haven't come easily to me, but I hope once I start practicing the experience will help me along. I will do a 3 part series on the approach to volume disorders.
Hopefully they will help you in your basic understanding.
Fluid Compartments:
For the fluid compartments think 60-40-20!
TBW is 60% of body wt (50% for women)
ICF is 40% of body wt
ECF is 20% of body wt
What are 3 reasons for oliguria?
1. low blood flow to kidneys
2. kideny problem
3. post-renal obstruction (need a Foley cath!)
*TBW = total body water
Source: Step up to Medicine (Agabegi and Agabegi)
Fluid Compartments (Normal)
Assessing Volume Status
Fluid Replacement Therapy
Hopefully they will help you in your basic understanding.
Fluid Compartments:
- Men and women are different. Men: TBW* = 60% of body weight, Women: TBW = 50%
- % of TBW decreases with age and increases with obesity (Why? Fat contains little water)
- How is water distributed?
- Intracellular (ICF) = 2/3rd of TBW (the largest proportion of TBW = skeletal muscle mass)
- Extracellular (ECF) = 1/3 of TBW
- Interstitial fluid = 1/3 of ECF
- Plasma = 2/3 of ECF
- Water exchange:
- Intake (normal) = 1500mL PO fluids, 500mL in solids/oxidation PER DAY
- Output (normal) = 800-1500mL in urine daily is normal
- 600-900mL per day is from insensible losses (variable bases on fever, trachs, hyperventilation, etc)
- 250mL lost in stool
- MIN OUTPUT per day = 500-600mL assuming normal kidney function
- Fluid shifts are based on hydrostatic and oncotic pressures (pull out your physiology book for a refresher in this)
For the fluid compartments think 60-40-20!
TBW is 60% of body wt (50% for women)
ICF is 40% of body wt
ECF is 20% of body wt
What are 3 reasons for oliguria?
1. low blood flow to kidneys
2. kideny problem
3. post-renal obstruction (need a Foley cath!)
*TBW = total body water
Source: Step up to Medicine (Agabegi and Agabegi)
8.12.2012
Asthma Charts
Every PACK-RAT I've taken has had at least 1-2 questions on asthma. During my primary care, pediatrics, and emergency medicine rotations I keep these charts with me because I used them daily.
Source: http://www.rtmagazine.com/issues/articles/2009-05_01.asp, http://www.uspharmacist.com/content/c/10133/?t=men%27s_health,otc_medications
Source: http://www.rtmagazine.com/issues/articles/2009-05_01.asp, http://www.uspharmacist.com/content/c/10133/?t=men%27s_health,otc_medications
8.08.2012
Reading a Chest Xray
You should feel confident reading a chest x-ray (CXR). It is one of the few films that will follow you from rotation to rotation. It doesn't matter if it is pediatrics, internal medicine, or surgery - You need to know how to read a CXR. Below are a couple sources to choose from because not everyone teaches or learns this in the same way. Here are a couple tips that I learned during my rotations from studying, my preceptors, or just plain screwing up!
- The first thing you should check is the name/date/type of film! (On one of my rotations, an intern (1st yr resident) was asked to read a chest X-ray for one of our patients who had just gotten a chest tube placed. He did a great job with lung pathology and describing the fluid - and he was also able to pick out that the chest tube was perfectly placed. I was impressed until the chief resident said "great job, you just harmed your patient." The chief had purposefully put up a CXR from 2 years ago when the pt had rec'd another chest tube. He then pulled up the current CXR to reveal that the tube was improperly placed. )
- Read every film in the same order every time.
- Learn the anatomy of what you are reading.
University of Washington's Method
1. PA or AP, supine or upright
2. Pt rotated? Check for vertebral and clavicle symmetry.
3. Lung volumes
4. Tube & line placement
- ETT 3-5 cm above carina
- NGT in stomach
- FT in stomach/duodenum
- Central line in SVC/R atrium
- Swan in PA
5. Pneumothorax: check apices on upright film, deep sulcus sign at bases
6. Pleural effusion, pleural thickening
7. Mediastinum: normal contour, wide
8. Heart: normal size, cardiomegaly
9. Lung parenchyma: masses, opacites, look for silhouette sign
10. Soft tissues: foreign bodies, SQ air, breast shadows
11. Bones: fractures, osteopenia, abnormalities
Silhouette Sign = obscuring of normal borders on radiograph caused by intrathoracic lesion.
Obscured R heart border = R middle lobe
Obscured L heart border = Lingula
Obscured diaphragm = Lower lobe
7.11.2012
ANKLE-BRACHIAL INDICES
ANKLE-BRACHIAL INDICES (ABI)
Indications: Presence of peripheral arterial disease
Technique
1. Have patient in supine position so arms, legs and heart are at same level.
2. Use blood pressure cuff and Doppler to measure systolic BP in both arms and record.
3. Use Doppler to identify location of dorsalis pedis and/or posterior tibialis pulses, mark location bilaterally.
4. Wrap BP cuff around lower leg. Using Doppler to listen to signal, inflate cuff until signal disappears, then slowly deflate until pulse signal returns. Record pressure at which pulse is heard (systolic) by Doppler at DP and PT in both ankles.
5. To calculate the AAI divide the highest SBP from each ankle (either DP or PT) by the highest SBP reading from the upper extremities.
6. ABI = ankle / arm systolic pressure
> 1.3 = suggests noncompressible, calcified vessels
0.91-1.3 = normal
0.41-0.9 = mild to mod peripheral arterial dz (range for claudication)
<0.4 = Severe peripheral arterial dz. (range for critical leg ischemia and rest pain)
Source: http://students.washington.edu/aomega/procedures.shtml#chestTube
Indications: Presence of peripheral arterial disease
Technique
1. Have patient in supine position so arms, legs and heart are at same level.
2. Use blood pressure cuff and Doppler to measure systolic BP in both arms and record.
3. Use Doppler to identify location of dorsalis pedis and/or posterior tibialis pulses, mark location bilaterally.
4. Wrap BP cuff around lower leg. Using Doppler to listen to signal, inflate cuff until signal disappears, then slowly deflate until pulse signal returns. Record pressure at which pulse is heard (systolic) by Doppler at DP and PT in both ankles.
5. To calculate the AAI divide the highest SBP from each ankle (either DP or PT) by the highest SBP reading from the upper extremities.
6. ABI = ankle / arm systolic pressure
> 1.3 = suggests noncompressible, calcified vessels
0.91-1.3 = normal
0.41-0.9 = mild to mod peripheral arterial dz (range for claudication)
<0.4 = Severe peripheral arterial dz. (range for critical leg ischemia and rest pain)
Source: http://students.washington.edu/aomega/procedures.shtml#chestTube
3.31.2012
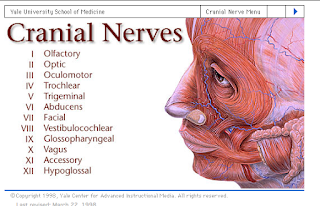
Cranial n. Learning Resource
Thanks for all of the views (10,000+), comments, and emails! Keep them coming and I will do my best to post information on the requested topics! Here is the most recent request:
3.29.2012
Causes of Secondary Hypertension
I am currently on my Ambulatory Medicine rotation at a hospital that sees a patient population primarily comprised of the homeless, imprisoned, and uninsured. The staff is incredibly nice and I'm loving my time there. Every week I am assigned a couple of topics to look up and present orally to the attending. I thought I would share my findings on each topic.
Ambulatory Topic #1: Causes of Secondary Hypertension
1.
Primary
renal disease — Both acute and chronic kidney disease,
particularly with glomerular or vascular disorders.
*You see elevated serum Cr concentration and/or an
abnormal urinalysis.
2.
Oral
contraceptives — Oral contraceptives typically raise the BP within the normal range but can also induce overt hypertension.
3.
Drug-induced
— Long term use of NSAIDs + many antidepressants can induce HTN.
Chronic ETOH intake and ETOH abuse can also raise blood pressure.
4.
Pheochromocytoma
— About 1/2 of patients with a "pheo" have paroxysmal HTN,
most of the rest have what appears to be primary HTN.
* You see:
-paroxysmal elevations in blood pressure
(which may be superimposed upon stable chronic hypertension)
-triad of headache (usually pounding),
palpitations, and sweating
-drug-resistant hypertension and those with
an adrenal incidentaloma should be evaluated for pheochromocytoma. Patients
identified with pheochromocytoma are rarely asymptomatic.
5.
Primary
aldosteronism — The presence of
primary mineralocorticoid excess, primarily aldosterone, should be suspected in
any patient with the
*You see:
-triad of hypertension, unexplained
hypokalemia, and metabolic alkalosis. However, some patients have a normal
plasma K+ concentration.
-otherwise unexplained or easily provoked
hypokalemia due to urinary potassium wasting.
->1/2 pts =normal serum K+
concentration.
-suspected in the presence of slight
hypernatremia, drug-resistant hypertension, and/or hypertension with an adrenal
incidentaloma
6.
Renovascular
disease — Renovascular disease = common disorder,
occurring primarily in patients with generalized atherosclerosis.
7.
Cushing's
syndrome — HTN is a major cause of morbidity +
death in pts with Cushing's syndrome.
-Cushing's syndrome (including that due to
glucocorticoid administration) is usually suggested by the classic physical
findings of cushingoid facies, central obesity, proximal muscle weakness, and
ecchymoses.
-Cushing’s or subclinical Cushing’s
syndrome should also be suspected in patients with drug-resistant hypertension
and in those with an adrenal incidentaloma.
8.
Other
endocrine disorders — Hypothyroidism, hyperthyroidism, and
hyperparathyroidism
-HTN may be associated with both
hypothyroidism, which may be suspected because of suggestive symptoms or an
elevated serum TSH level, and primary hyperparathyroidism. The latter is most
often suspected because of otherwise unexplained hypercalcemia, which may
affect vascular reactivity, day-night blood pressure regulation, and renal
function
9.
Obstructive
sleep apnea — Disordered breathing during sleep appears to
be an independent risk factor for systemic hypertension.
-sleep apnea syndrome is most commonly
identified in obese men who snore loudly while asleep. These patients have
repeated apneic episodes at night due to passive collapse of the pharyngeal
muscles during inspiration, such that the airway becomes occluded from the
apposition of the tongue and soft palate against the posterior oropharynx.
-A variety of other symptoms may be seen
including headache, daytime somnolence and fatigue, morning confusion with
difficulty in concentration, personality changes, depression, persistent
systemic hypertension, and potentially life-threatening cardiac arrhythmias.
-Patients with obstructive sleep apnea
often retain sodium and fail to respond optimally to antihypertensive drug
therapy
10.
Coarctation
of the aorta — Coarctation of the aorta is one of the major
causes of secondary hypertension in young children
-Coarctation of the aorta is one of the
major causes of secondary hypertension in young children but may first be
detected in adulthood (picture 1A-B). The classic findings are HTN in the upper
extremities, diminished or delayed femoral pulses ("brachial-femoral
delay"), and low or unobtainable arterial blood pressure in the lower
extremities. In addition, a prominent “to-and-fro machinery murmur” from the
aorta may be heard over the posterior chest.
Source: uptodate.com
Pic:http://www.aakp.org/aakp-library/ped-hypertension/
Pic: http://www.angiologist.com/secondary-hypertension/
3.27.2012
Nephrolithiasis - When Should I Admit?
I recently had a patient who came in complaining of severe
flank pain radiating to his groin with nausea and vomiting… it was determined
that he had nephrolithiasis (kidney stones). My attending asked me whether or
not we should admit the patient… Good question, I thought. I was able to rattle
off the text book treatments, but I wasn’t clear on the guidelines for
admission vs. out-patient treatment. Below is an overview of treatment
including some clear indications for admission.
General Treatment (for all types of stones):
1-PAIN CONTROL!
a-PO analgesic or IV morphine,
situation dependent
b-Parenteral NSAID (Ketorolac)
2-Hydration (vigorous)
3-Antibx, if UTI present
Additional treatment measures based on pain severity:
MILD-MOD pain = high fluid intake, oral
analgesics, wait for stones to pass (Give pt a urine strainer because you want
to know what “kind” of stone the patient has.)
SEVERE pain = IV fluids and pain control, KUB,
IVP to find site of obstruction, consult urology (surgery) if stones do not pass
in 3 days
ONGOING pain w/o relief from narcotics =
Surgery
Types of Surgery (10,000 foot view):
Shock wave lithotripsy: most common, it breaks
apart the larger stones so they can be passed spontaneously, typically used for
stone >5mm and < 2cm
Percutaneous nephrolithotomy: used if the
above fails, if stones are > 2cm, for struvite stones
Admission is indicated if:
1-Oral analgesics
are insufficient to manage the pain.
2-Ureteral
obstruction from a stone occurs in a solitary or transplanted kidney.
3-Ureteral
obstruction from a stone occurs in the presence of a urinary tract infection
(UTI), fever, sepsis, or pyonephrosis.
4-Large stones
(>1cm)
*The above
indications were found in a couple of sources, but more say that the ultimate
decision is made on a clinical basis, not solely on guidelines.
Parting suggestion: brush up on the different kinds of
kidney stones
Sources:
Medscape: Nephrolithiasis and Treatment, http://emedicine.medscape.com/article/437096-treatment
Step Up to Medicine 2nd Ed. by Agabegi and
Agabegi
Picture: http://knol.google.com/k/kidney-stones#
3.11.2012
Treating Hyponatremia in the ED
After reading this blog entry from EM CRIT BLOG I felt better regarding the treatment of hyponatremia so I thought I would share. This blog has some great information and most blogs have a podcast option.
"In this podcast, I discuss the management of hyponatremia in the ED. After reading countless articles from the nephrology literature…I can still attest that I have not a friggin’ clue about renal physiology. But I think I have found a simpler path to the work-up and treatment of low sodium in the ED."
3.10.2012
Levothyroxine vs Brand-Name
I vaguely remembered a comment from our endocrine teacher about not putting our patients on generic levothyroxine for hypothyroidism and that we should always opt for a brand name if the patient could afford it -- but the exact reason why had escaped me. I was recently presented with a situation in which I needed to make the call - generic vs brand - so I did some research and spoke to an endocrinologist. These are the main points that I came up with...
1. For tight control of TSH, use a brand name (which brand isn't important)
2. Tight control is particularly important in pregnant women, those looking to get pregnant, and those with h/o goiter or thyroid cancer
3. Once you pick a brand, try to stick to the same brand-name each month
4. The problem with generic levothyroxine is that the manufacturers producing the drug are variable and there are many companies moving in and out of the market so it is difficult to get the SAME generic pill each month from the pharmacy
5. If your pt can only afford generic, encourage them to take a photo of the pills that they get from the pharmacy - if they ever pick up their Rx and the pills look different then they should contact you to schedule thyroid blood work check in 5-6 weeks since the new generic could vary as much as 12.5%. If they are receiving the same generic pill each month, you should schedule normal follow ups. The bottom line is that each time they get a new generic pill from a new manufacturer, they should be re-tested.
This becomes important because many primary care providers Rx the generic because they believe that it isn't any different from brand names - and in most cases they are completely right. Ibuprofen vs Advil - no real noticeable clinical difference. The thyroid, however, is extremely sensitive and even the slightest variation from generic #1 to generic #2 can make someone's TSH impossible to tightly control and may even make them thyroid toxic.
When I presented this to several PCPs, it was received with a lot of skepticism. The first question they all asked was "Who did the study, the drug companies?" A great question to ask. The answer is... in addition to drug company studies... there have been independent studies and results have been examined by the FDA, Endocrinologist Societies (world-wide), and the Thyroid Association - all are in agreement about the results. There is a ppt available describing the results of these studies. They show the bioequivalence of generic vs brand, but also demonstrate the vast variability between generic manufacturers.
If you are looking for a quick 1 page break down of this subject - check out the following: Hennessey JV. Levothyroxine dosage and the limitations of current bioequivalence standards
3.09.2012
Thyroid Resource
3.03.2012
OB/GYN Study Sources
I have had a few people ask me which books I used to prepare for my OB/GYN rotation so I thought it would be a good idea to share with everyone. The 4 main sources that I used to study before/during my rotation are:
1. Blueprints: OB/GYN ($35-40)
2. Case Files: OB/GYN ($25-30)
3. Obstetrics, Gynecology, and Infertility (Great pocket guide) ($15)
4. UpToDate.com (which I can only use at the hospital because I do not have a personal subscription)
I wanted to share a little about the Case File series because although I had heard of them before, I hadn't used them -- but now that I have - I love the set up. Each chapter starts with a brief case vignette and a couple questions such as: What is the likely diagnosis? or What would you do next? Then you are given the answers along with a brief teaching section on the topic. Lastly, they give you 5 or so multiple choice questions covering the chapter material (answers included). By the end of each chapter I really felt like I knew the material. This set up may not be for everyone so I took some page-shots so you can check it out before you make the purchase. I borrowed mine from the school library for the duration of my rotation.
1. Blueprints: OB/GYN ($35-40)
2. Case Files: OB/GYN ($25-30)
3. Obstetrics, Gynecology, and Infertility (Great pocket guide) ($15)
4. UpToDate.com (which I can only use at the hospital because I do not have a personal subscription)
I wanted to share a little about the Case File series because although I had heard of them before, I hadn't used them -- but now that I have - I love the set up. Each chapter starts with a brief case vignette and a couple questions such as: What is the likely diagnosis? or What would you do next? Then you are given the answers along with a brief teaching section on the topic. Lastly, they give you 5 or so multiple choice questions covering the chapter material (answers included). By the end of each chapter I really felt like I knew the material. This set up may not be for everyone so I took some page-shots so you can check it out before you make the purchase. I borrowed mine from the school library for the duration of my rotation.
Subscribe to:
Posts (Atom)